Sacroiliac Joint Pain - How Do I Help My Patients?
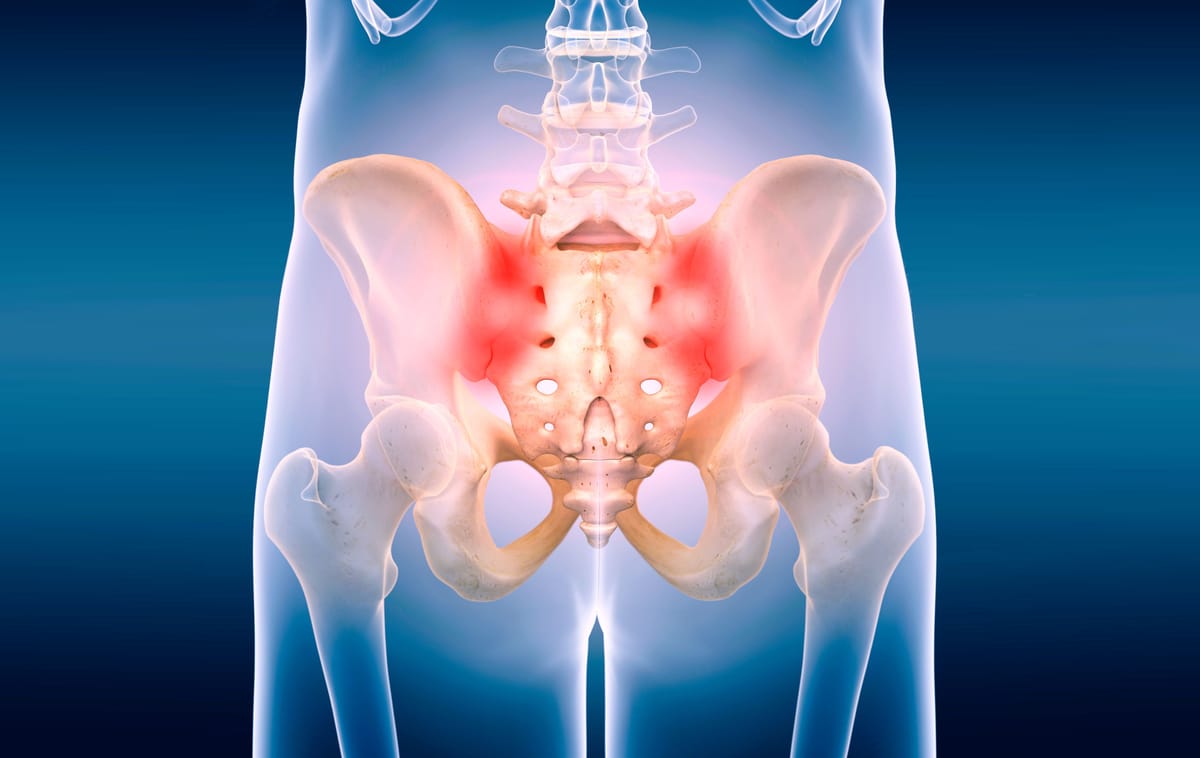
Sacroiliac (SI) joint pain is a common but challenging source of low back pain, affecting 16-30% of sufferers. Explore evidence-based approaches to effectively manage SI joint pain in patients, ensuring better outcomes with a step-up treatment strategy
Introduction
So... this ended up being a long one - apologies in advance but hopefully it's helpful for one set of those patients who we find more difficult to diagnose and know what to do with!
Sacroiliac (SI) joint pain is a common cause of reported low back pain. In cases of low back pain it is estimated that between 16% and 30% of these will be due to sacroiliac joint pain/dysfunction. The actual cause of the pain is often unknown unless ligamentous injuries (rare) or fractures (rarer) are present.
Localised tenderness to the SI joint is often considered one of the most common features of this condition but what should you be looking out for in clinic and what does the evidence based treatment for this condition look like? You might have heard about nerve blocks being the gold standard of differential diagnosis also but are these really practical and needed for every patient?
Let's go!

Patient Assessment
Subjective assessment
Detailed patient history (as always) is crucial and will form an important part of the diagnosis. As a minimum consider the following points:
-
The age of the patient, because many conditions occur within certain age ranges (ankylosing spondylitis versus osteoarthritis)
-
The acuteness or chronicity of the pain. Was there an acute traumatic injury or a chronic repetitive injury?
-
The mechanism of any injury
-
For active pregnant women, remembering that pregnancy causes laxity of the SI joint and predisposes women to pain or injury
-
The quality and intensity of the pain as well as any radiation or referred pain (usually unilateral, dull, and deep, with radiation to buttock, posterior thigh, or groin).
-
Previous low back injuries, with the treatments and outcomes.
-
The presence of red flags signalling more serious pathology

Objective assessment
So this is a hard one. Here mainly you are looking to exclude other pathology such as a hip related cause or a lumbar related cause so a thorough assessment of these areas is always a good idea, however the subjective history will tend to be your friend in terms of guiding towards an impression as to what is going on and if it is SI joint pain.
Palpation whilst this can be reassuring for the patient as they tend to feel more examined (get subscribed for a post on this soon) is if limited diagnostic value but if there is pain present on palpation can be a good indicator coupled with your subjective findings.
The literature here shows limited diagnostic value in many of the special tests we would traditionally look to use in isolation e.g. stork test, FABER test, Mekhail test. However (as is becoming more and more common) when we look at a cluster of tests then we an increase the sensitivity and therefore increase their usefulness dramatically.
For SI joint pain the use of the Mekhail and FABER tests together gives us a sensitivity of over 90% but it does make the result less specific with only 17% of negatives screen out correctly.
There is other more anecdotal evidence that the use of any of the special tests that look at stressing the SI joint when used as a cluster are pretty good but no numbers are provided in the literature in terms of specificity and sensitivity. I would take this as a 'do a cluster rather than a single test and if all positive then you are likely on the right lines' approach.
So what does that mean? Concentrate on your history taking! It will really give you a good indication of if it is likely to be SI joint pain and then use the Mekhail and FABER tests together to look to rule in rather than exclude. Positive tests with positive history = very likely!
Imaging
While X-ray and MRI scans can help rule out other causes of pain, their role in diagnosing SI joint dysfunction is limited as often despite the patient having the pain, imaging will be 'normal'. So can we use this inversely like in frozen shoulder to rule it in if negative? No. Think about a mechanical low back pain, that will also often come back 'normal' on imaging so it won't help your diagnosis.
Imaging, however, can be helpful in ruling out fracture and MRI may help to rule out discogenic pain (but isn't in keeping with NICE guidance for this).
Diagnostic SI joint injections/nerve blocks can provide both diagnostic and therapeutic benefits by confirming the SI joint as the pain source but obviously this would necessitate referral into secondary care and as conservative management is a good first line treatment approach then this would be overkill in the first instance. Having said that most of the literature looks at this as the gold standard for diagnosis so in chronic patients this may be a good referral option to look at diagnosis and treatment.

Management/Treatment Options
Treatment of SI joint pain typically involves coming at the condition from different angles and promoting movement whilst controlling pain. Obviously if there is a cause for the SI joint pain such as dislocation or fracture then treatment of this is the go to. Otherwise here are the good evidence based treatment approaches:
Exercise based management: Tailored exercises to strengthen the core and pelvic muscles and also targeting the lumbar spine with a focus on improving flexibility, and enhancing joint stability have good evidence of improving pain and function
Pain Management: NSAIDs mainly to manage pain and inflammation (if tolerated) and consider another analgesic such as paracetamol to allow good pain control to promote movement and adherence to home exercise plans
Corticosteroid injections: These can reduce inflammation and provide significant pain relief but very short term. If very acute pain with absence of red flags again may help to improve function and get a handle on pain whilst undergoing other treatment approaches
Radiofrequency Ablation (RFA): This minimally invasive procedure uses heat to disrupt nerve function and alleviate chronic pain there is limited evidence for it's effectiveness for SI joint pain but there are limited studies on it in this population so likely needs further study. This may be offered to the patient by pain management services.
There is also the surgical option of SI joint fusion. There is a lot of evidence that this will improve pain but obviously comes with all the usual risks of surgery so these patients should be carefully selected and will need a confirmed diagnosis of SI joint pain (this is achieved with the gold standard of a guided nerve block - if it relieves pain then this is positive). It also isn't 100% 'curative' so is often seen as a last report for patients who have more chronic pain.

Adjuncts and Their Evidence
Acupuncture: Some studies suggest acupuncture may provide pain relief and improve function in patients with SI joint pain, though evidence is mixed and further research is needed
Prolotherapy: This regenerative injection technique aims to strengthen ligaments and has shown promise in small studies, but larger trials are needed to confirm its efficacy
Manual Therapy: Manual therapy especially in the form of manipulation of the SI joint/s have shown benefits in some patients, particularly when combined with other treatments
Key Takeaways

- Subjective assessment needs to be thorough as it forms the basis of the diagnosis
- Ask about pregnancy! - much more common in pregnant women or those who have recently given birth due to ligament laxity
- Rule out red flags, lumbar spine causes, radicular causes and inflammatory pathology
- Objective assessment findings are useful but need to consider them in the context of the subjective assessment and use to conform your impression rather than rule out
- Special tests are more useful when used as a cluster and there is evidence for FABER and Mekhail test
- Imaging isn't useful unless ruling out other serious pathology
- Treatment options are largely conservative and look at it as a step up approach, in primary care especially, start with exercises and optimising pain relief and then move on to potential referrals into secondary care as appropriate
- Treatment evidence is mixed with a lot of low quality studies for everything other than exercise based management and injections
- Chronic pain can be managed with surgical intervention as a last resort