Osteoporosis - What can we do?
FCPs are well positioned with longer appointments to address issues that involve lifestyle modification advice but also the evidence shows most of this group of patients will present after a fragility fracture so they will present often with pain/needing MSK management so would be streamlined to us.

Osteoporosis is an age-related metabolic disease which primarily impacts bone and causes demineralisation of this bone. This results in a weakening of the bone and makes it more prone to fractures. It is most common in postmenopausal women and is classed as a 'serious yet preventable' disease. Lifestyle modification is one of the most significant steps that can be taken to lower the risk factors and increasing weight-bearing physical activity is one of the easiest steps to take as part of this.
It is a serious public health concern around the world and has even been linked with increased mortality in individuals affected. 1 in 3 women worldwide are at risk of suffering a fragility fracture related to osteoporosis. This is an alarming statistic when the research still says that osteoporosis is underdiagnosed and undertreated.

NICE advocates that primary care in general should be taking a lot more of the lead on the identification of these patients but I think FCPs are uniquely positioned to help with this. Why? Well, let's go through the factors, how to lower the risk and then why I think we should help.
TL;DR - FCPs are well positioned with longer appointments to address issues that involve lifestyle modification advice but also the evidence shows most of this group of patients will present after a fragility fracture so they will present often with pain/needing MSK management so would be streamlined to us. Exercise is also something (I hope!) we know something about and can give advice on.
Recognition
NICE guidance recommends assessing the fracture risk in all women aged 65 years and older and all men aged 75 years and older using a validated tool such as FRAX or QFracture.
It then goes on to say that if they trigger on these scores then consider something like a DEXA scan and not just DEXA in the first instance
What about younger people? - Screen these if they have risk factors that would increase their risk of a fragility fracture

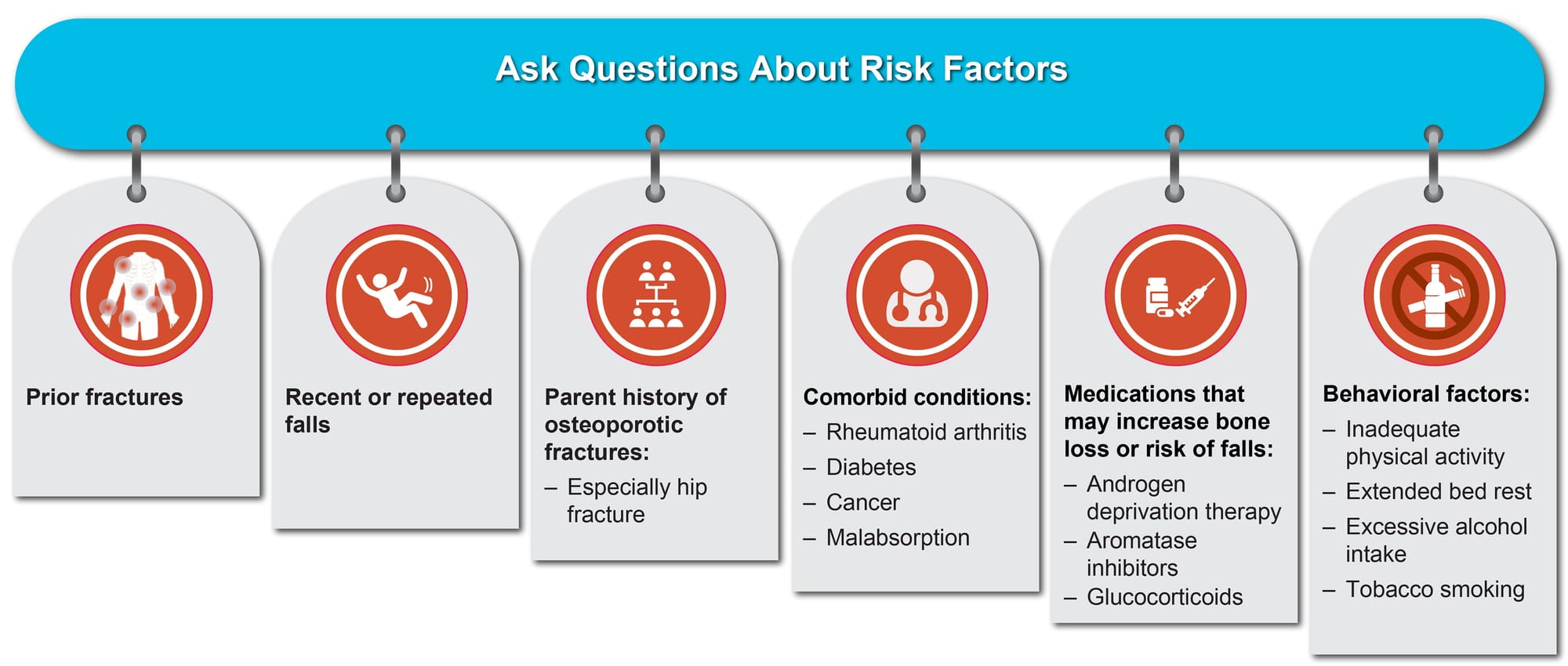
These risk factors are:
- Previous fragility fracture
- Current or frequent recent use of glucocorticoids (e.g. prednisolone and dexamethasone)
- History of falls
- Family history of hip fracture
- Low BMI
- Smoking
- Alcohol intake of more than 14 units per week
There are also many conditions which can cause secondary osteoporosis - see my other article which breaks these down HERE
When using a tool such as FRAX to assess the risk of fragility fracture then we need to take into account that these do have a couple of limitations such as underestimating the risk of fracture in people who have a history of multiple falls, have had previous vertebral fractures, have a high alcohol intake and people aged over 80.
FRAX Tool
Available HERE
- Need to know the patient's BMI
- Calculated using the BMI, number of risk factors and age
- It then gives you a 10-year probability of fracture and you can even get this interpreted for you based on the National Osteoporosis Guidelines!
- Can then add DEXA result for more accuracy (if it was indicated)
QFracture
Available HERE
- Another questionnaire-based tool
- Advantageous over FRAX in the UK if no DEXA result as it is more extensively validated
- Predicts fracture risk over a wider age range, in elderly populations and in ethnic groups more accurately
- Seen as better to use if you don’t have a DEXA result
- Simplest way to remember - QFracture is normally better unless you have a DEXA then do FRAX and use the DEXA result
DEXA Scan Result

- Higher is better
- Normal is anything above a T-score of -1.0
- Osteopenia = between -1.0 and -2.5
- Osteoporosis = -2.5 and below
Lowering the risk
See those risk factors above? Well, we can help patients to understand that these are risk factors and modify them! I’m going to discuss some simple ways to make a difference below but there are loads of others so feel free to share advice in the comments!
This can be as simple as offering patients something as simple as a falls risk assessment when they present to you having had a fall or asking about falls at home for patients who present as less steady on their feet and then giving simple preventative advice. One such source for this is the Chartered Society of Physiotherapy here
Exercise is a major preventative factor and increasing this in general in the population is effective in lowering the risk of and preventing many different conditions. For Osteoporosis it is recommended that both weight-bearing exercise (e.g. walking) is increased alongside strength training as studies have shown strength training increases bone mineral density.

HRT is also effective in reducing the risk of Osteoporotic fractures as Osteoporosis is more prevalent in post-menopausal women and it is thought that the reduction in oestrogen causes an increase in the rate of bone reabsorption relative to the rate of new bone formation. Therefore offering HRT and reviewing HRT are good ways of decreasing risk.
Diet! Again a fairly easy conversation to have and an effective one! Did you know that green leafy vegetables such as kale are a great source of calcium? Fortified plant milk or cow's milk are also great sources so often having the conversation and signposting to advice on calcium is an effective intervention before any Adcal or similar supplementation or alongside.
Why we can (and should) help as FCPs
Simples - we usually have 20-minute appointments and often are already asking about some of the risk factors such as trauma, fractures, falls and general activity levels. Simply having an awareness of how these fit into Osteoporosis risk factors is a great start!
Given osteoporosis is underdiagnosed these patients will often present after a fragility fracture. These patients will present with MSK pain so (should) be streamlined to FCP. Assessing for osteoporosis risk at this stage is something that we can do and can have a real positive impact on preventing further fractures.
Then look at the section on lowering risk above… how often are we advising regarding exercise? Why don’t you simply offer advice about increasing general exercise but in a way that will be beneficial for bone health such as higher intensity weight-bearing exercise or increasing the amount of strength-building exercise?
We are also in a great position to complete a FRAX or QFracture. These are simple questionnaire-based risk assessment measures that can be carried out by any health professional. Identifying that someone is at risk then allows the risk factors to be addressed and a DEXA carried out if necessary. Yes, you might not be in a position to prescribe bone protection or refer for the DEXA but by completing the risk assessment it allows you to start conversations about the risk factors and preventative measures and allows for a more focused referral back to the GP to consider DEXA and bone protection as required.

FCPs are really well placed to have a good impact on reducing the risk of osteoporotic fractures through addressing bone health and this allows for effective use of resources in primary care and a good use of FCPs reducing the GP workload and is also part of QOF. QOF is an annual reward and incentive programme for GPs in England which allows for an additional funding stream so your practices will be happy too as they try to hit as many of the QOF indicators are possible each year!
References and Further Reading
Jarrell, L. (2023). Osteoporosis management in primary care. The Nurse Practitioner, 48: 11.
Nguyen, VH. (2017). Osteoporosis prevention and osteoporosis exercise in community-based public health programs. Osteoporosis and Sarcopenia, 3: 18–31.
NICE. (2012). Overview | Osteoporosis: assessing the risk of fragility fracture | Guidance | NICE Available: https://www.nice.org.uk/guidance/cg146 [Accessed: 2/3/2024].
NICE. QOF indicators | Goals and outcome measures | Osteoporosis - prevention of fragility fractures | CKS | NICE Available: https://cks.nice.org.uk/topics/osteoporosis-prevention-of-fragility-fractures/goals-outcome-measures/qof-indicators/ [Accessed: 22/4/2024].
Otero, M, Esain, I, González-Suarez, ÁM, Gil, S. (2017). The effectiveness of a basic exercise intervention to improve strength and balance in women with osteoporosis. Clinical Interventions in Aging, Volume 12: 505–513.
Plawecki, K, Chapman-Novakofski, K. (2013). Effectiveness of Community Intervention in Improving Bone Health Behaviors in Older Adults. Journal of Nutrition in Gerontology and Geriatrics, 32: 145–160.
QFracture Available: https://qfracture.org/ [Accessed: 22/4/2024].
Royal Osteoporosis Society - Better Bone Health for Everybody Available: https://theros.org.uk/ [Accessed: 22/4/2024].
Shin, YH, Hur, HK, Pender, NJ, Jang, HJ, Kim, M-S. (2006). Exercise self-efficacy, exercise benefits and barriers, and commitment to a plan for exercise among Korean women with osteoporosis and osteoarthritis. International Journal of Nursing Studies, 43: 3–10.
Singer, AJ, Sharma, A, Deignan, C, Borgermans, L. (2023). Closing the gap in osteoporosis management: the critical role of primary care in bone health. Current Medical Research and Opinion, 39: 387–398.
Sobh, MM, Abdalbary, M, Elnagar, S, Nagy, E, Elshabrawy, N, Abdelsalam, M, Asadipooya, K, El-Husseini, A. (2022). Secondary Osteoporosis and Metabolic Bone Diseases. Journal of Clinical Medicine, 11: 2382.