Corticosteroid Injections in Primary Care: Overview of Uses and Risks
Explore the increasing use of corticosteroid injections in primary care for managing musculoskeletal conditions like osteoarthritis. Understand their indications, potential risks such as post-injection flare and systemic effects in this quick overview!

Introduction
In recent years, the use of corticosteroid injections in primary care has been on the rise. These injections are commonly used to treat a variety of musculoskeletal conditions, providing relief from pain and inflammation. This blog post explores the reasons behind this increase, as well as the benefits and risks associated with corticosteroid injections.
Why is Corticosteroid Injection Use Increasing?
Increased Prevalence of Musculoskeletal Conditions
One of the primary reasons for the increased use of corticosteroid injections is the rising prevalence of musculoskeletal conditions, such as osteoarthritis, tendinopathy, and bursitis. Since these conditions are frequently seen in aging populations and become more prevalent with increasing age, it follows that as the population ages, the incidence of these conditions will also increase.
Effectiveness in Pain Management
Corticosteroid injections are known for their effectiveness in managing pain and inflammation. They often provide rapid relief, which can be particularly beneficial for patients who have not responded well to other treatments. This enables them to continue treatments such as exercises, and studies show this combined approach is particularly beneficial for many conditions like Osteoarthritis. Therefore, these are components of evidence-based guidelines and shared decision-making tools for these health issues.
Avoidance of Surgery
For many patients, corticosteroid injections offer a non-surgical alternative to managing their conditions. This is especially important for those who may not be suitable candidates for surgery because of age, comorbidities, or personal preference. They can often also be used to 'bridge the gap' between referral for surgical intervention and the actual surgery.
Benefits of Corticosteroid Injections

Rapid Pain Relief
Corticosteroid injections can provide quick relief from pain and inflammation, often within a few days of the injection. This can help patients return to their daily activities more quickly, which can be particularly important for many patients who need to return to work e.g. in a manual job as they are self employed.
Reduction in Inflammation
These injections help reduce inflammation in the affected area, which can improve function and mobility. This proves beneficial in cases of rheumatoid arthritis, although most corticosteroid injections given specifically for this purpose are done in specialist clinics rather than in Primary Care.
For soft tissue inflammation, such as in patients with tendinopathy, research has also shown that whilst there is a good short-term benefit to reduction of inflammation in tendinopathy, most show a negative response longer term.
Delaying or Avoiding Surgery
By providing effective symptom relief, corticosteroid injections can help delay or even avoid the need for surgical interventions. This can be a significant advantage for patients looking to avoid the risks and recovery time associated with surgery.
It is also more frequently becoming the case that corticosteroid injections are trialled even as a 'stop-gap' whilst the patient is on the surgical waiting list (e.g. in Osteoarthritis management) as the waiting list for surgery is so long.
Risks of Corticosteroid Injections

As with any drug, there are risks and potential side effects. Below, we have tried to summarise the main ones and provide some context with incidence rates (where known/studied). All references are provided at the end of the post. The primary references for the incidence rates are Risk Management in Soft Tissue and Joint Injections document from the CSP and Local and Systemic Side Effects of Corticosteroid Injections for Musculoskeletal Indications from the American Journal of Roentgenology
These will be considered in more detail in a further blog post including some information you can use for patients so subscribe to be notified!
Local Side Effects
- Immediate Onset (within 48 hours)
- Postinjection Flare: Exacerbation of pain post-injection, more common with particulate corticosteroids. Incidence: 8% 1.
- Delayed Onset (after 48 hours)
- Skin Hypopigmentation and Atrophy: Particularly after superficial injections, usually resolving within a year. Incidence: 9% 1.
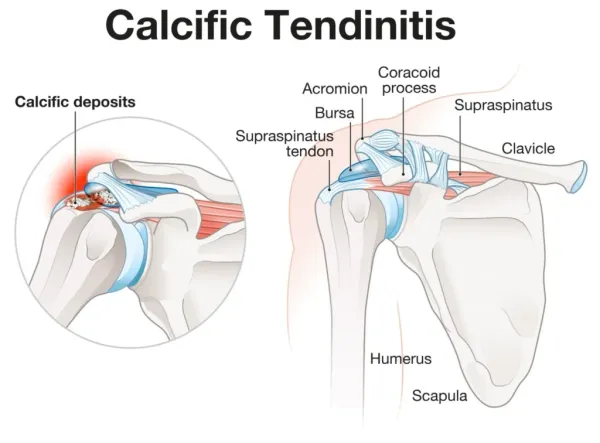
- Soft-Tissue Calcification: Can cause increased pain and may be clinically significant. Incidence: Rare 2.
- Infection: Rare but possible, with higher risk if surgery follows soon after injection. Incidence: <0.001% 2.
- Tendon Rupture: Rare but significant, with higher risk in tendons under biomechanical stress. Incidence: 0.1% 1.
- Accelerated Progression of Osteoarthritis: Increased joint space loss and radiographic progression. Incidence: Varies 2.
- Osseous Injury: Includes insufficiency fractures, osteonecrosis, and rapid joint destruction. Incidence: 1% 2.
Systemic Side Effects
- Immediate Onset
- Facial Flushing: Common, especially in women, and self-limiting. Incidence: 40% 2.
- Hypertension and Hyperglycemia: Transient increases in blood pressure and blood sugar levels. Incidence: Common 2.
- Hypersensitivity Reactions: Rare but can include anaphylaxis. Incidence: 0.3-0.5% 2.
- Ophthalmic Conditions: Can exacerbate glaucoma or cause chorioretinopathy. Incidence: Varies 2.
- Delayed Onset
Special Considerations
- Premenopausal Women: Hormonal suppression can cause menstrual irregularities. Incidence: 51% 2.
- Patients with Diabetes: Significant impact on serum glucose levels, requiring careful monitoring. Incidence: Common 2.
- Athletes: Risk of tendon weakening and adrenal insufficiency, advising against vigorous activity post-injection. Incidence: Varies 2.
- Paediatric Patients: Limited data, but potential for significant side effects like Cushing's syndrome. Incidence: 2.6% (skin hypopigmentation and atrophy) 2.
- Patients on Anticoagulation Therapy: Low risk of bleeding, but guidelines suggest no need to discontinue therapy. Incidence: Low 2.
- Patients on Ritonavir: Risk of severe adrenal insufficiency because of drug interactions. Incidence: Varies 2.
Conclusion

Corticosteroid injections have become an increasingly popular treatment option in primary care because of their effectiveness in managing pain and inflammation.
Whilst effective for short-term pain relief, corticosteroid injections come with a range of potential side effects that need to be carefully considered and communicated to patients. By carefully considering the benefits and risks, corticosteroid injections can be a valuable tool in the management of musculoskeletal conditions but should always be considered as part of a shared decision-making approach and their effectiveness for individual conditions discussed with the patient.
It is also important to remember they are rarely a management option on their own for many conditions and therefore a combined treatment approach and knowledge of this is needed by both the treating clinician and the patient